If you are recovering from an addiction to drugs and alcohol, you know that the road to recovery is full of challenges. You have to manage cravings, stave off relapses, handle withdrawal symptoms, and rebuild relationships, among many other tasks. However, one of the most common and most stressful issues that people in recovery face is sleep disorders. Not being able to sleep can heighten your chances of relapse and make recovery even more difficult – but there are strategies you can use to manage your sleep and get the rest you need.
What Happens To Your Sleep In Recovery?
 According to the Journal of Addiction Medicine, people in recovery are 5 times more likely to suffer from insomnia than the general population. People in recovery are mainly at risk for these sleep disorders because of the complex psychological issues that occur when coming off of a substance, especially if you used this substance to help you fall asleep in the past. Sleep disorders can range during recovery – you may only deal with them during the withdrawal period, or you can keep experiencing them for weeks, months, or even years after recovery.
According to the Journal of Addiction Medicine, people in recovery are 5 times more likely to suffer from insomnia than the general population. People in recovery are mainly at risk for these sleep disorders because of the complex psychological issues that occur when coming off of a substance, especially if you used this substance to help you fall asleep in the past. Sleep disorders can range during recovery – you may only deal with them during the withdrawal period, or you can keep experiencing them for weeks, months, or even years after recovery.
When it comes to addiction, you can experience long-lasting effects that impact your physical and mental health. Anxiety, depression, and other psychological conditions contribute to insomnia – and these issues are also common side effects during the recovery process. Unfortunately, sleep disorders can also feed into the risk of relapse, making recovery even more difficult.
First, you may have used the substance you are recovering from to help you sleep in the past. Now that you are clean from this substance, you cannot rely on it to fall asleep. In addition, you may be battling with very unpleasant side effects while in recovery – anxiety, depression, stress, and fear are some of the most common. As a result, it is more difficult for you to fall asleep at night.
Since it is more difficult to fall asleep, the sleep disorder exacerbates some of your recovery side effects. In particular, insomnia makes anxiety, depression, and stress even worse. You feel irritable, overtired, and like you cannot perform your daily functions – and your stress levels go through the roof.
You may think that old coping mechanisms, such as drug and alcohol use, are looking like a better decision. Since you are suffering from sleep deprivation, you could have more impulsive tendencies and want to end your discomfort as soon as possible. You could run the risk of relapsing at this point, or you could continue to suffer from sleep issues. However, a third option is available: using healthy methods to improve your sleep.
How Does Addiction Impact Your Sleep?
While sleep disorders in recovery are common, it is likely that you have experienced trouble sleeping before. Addiction itself can worsen your sleeping habits. Depending on the type of substance you used, you could impact your brain chemistry and sleep cycles. In addition, addiction withdrawal symptoms can also reduce your quality of sleep.
Because of the changes that drugs and alcohol make to your body, it can be very difficult to develop healthy sleeping habits while on these substances. Recovery and healthy sleep methods are the best options.
Addiction throws your natural body clock out of its rhythm – you often stay up very late in the night and wake up very late in the day. Drugs can also impact the time you spend in REM sleep, which reduces your feelings of restfulness in the morning. It takes longer to fall asleep when you are addicted to a substance, and you will reduce your overall sleep time because you often wake up during the night.
Tips For Improving Sleep While In Recovery From Addiction
While sleep disorders are often unavoidable in addiction recovery, it doesn’t mean that you cannot get a good night’s sleep. Follow these tips to enjoy a better night’s sleep and naturally improve your symptoms:
- Exercise plays an important role in regulation your sleep cycles and increasing your relaxation during the day. In addition, exercise produces natural endorphins that can aid in your recovery journey. Performing 15 to 30 minutes of exercise about 3 to 4 hours before you go to bed can have a great impact on your ability to fall asleep.
- Meditation can also aid in helping you fall asleep, especially if anxiety or intrusive thoughts play a role in your insomnia. With consistent practice, you can reduce your stress and help you focus on the present, both of which can help you fall asleep easier.
- You can change your sleep environment to promote relaxation and aid you in falling asleep. If your mattress is uncomfortable, invest in a new one and supply it with supportive pillows, new blankets, and clean sheets. Keep your bedroom at a comfortable temperature, around 60 to 70 degrees Fahrenheit. Invest in a white noise machine to block out intrusive noises.
- Using electronic devices right before bed can make it harder to fall asleep, since the blue light can block the release of your sleep hormones. Enable night mode to lower your exposure to this light before bed or avoid screens completely in the hours before you fall asleep.
- A poor diet can also make it more difficult to get some rest, in addition to increasing stress and discomfort. Avoid foods that are high in sugar, fat, spice, and caffeine after midday. Incorporate foods that promote sleep, such as legumes, leafy green vegetables, dairy products, and meats, into your diet. Avoid eating large, heavy meals late at night.
- Establishing a regular bedtime routine can also help you fall asleep easier. Having a regular schedule allows you to develop a ritual that can help you combat insomnia and promote relaxation. Avoid doing anything other than sleeping and relaxing in your bed. Go to bed and wake up around the same times every day, including weekends. Perform relaxation activities before bed, such as meditating, doing some light yoga, taking a warm bath, or reading a book.
If you are still struggling from a sleep disorder during recovery, visit a medical professional as soon as possible. If you find yourself struggling with a sleep disorder due to addiction, seek professional treatment from a drug and alcohol rehabilitation center. For more information on pursuing your recovery journey, visit Echo Recovery today to gain valuable resources from others like you.

Experienced Chief Executive Addiction Recovery and Mental Health Professional
Business professional in the Addiction Recovery and Mental Health industry for the past 26 years. Caring, compassionate and strongly motivated to make a difference in the organizations I am affiliated with and welfare of the population we serve. Currently focused on advocating, educating and developing projects leveraging evidence based, real time technology to support individuals in recovery.


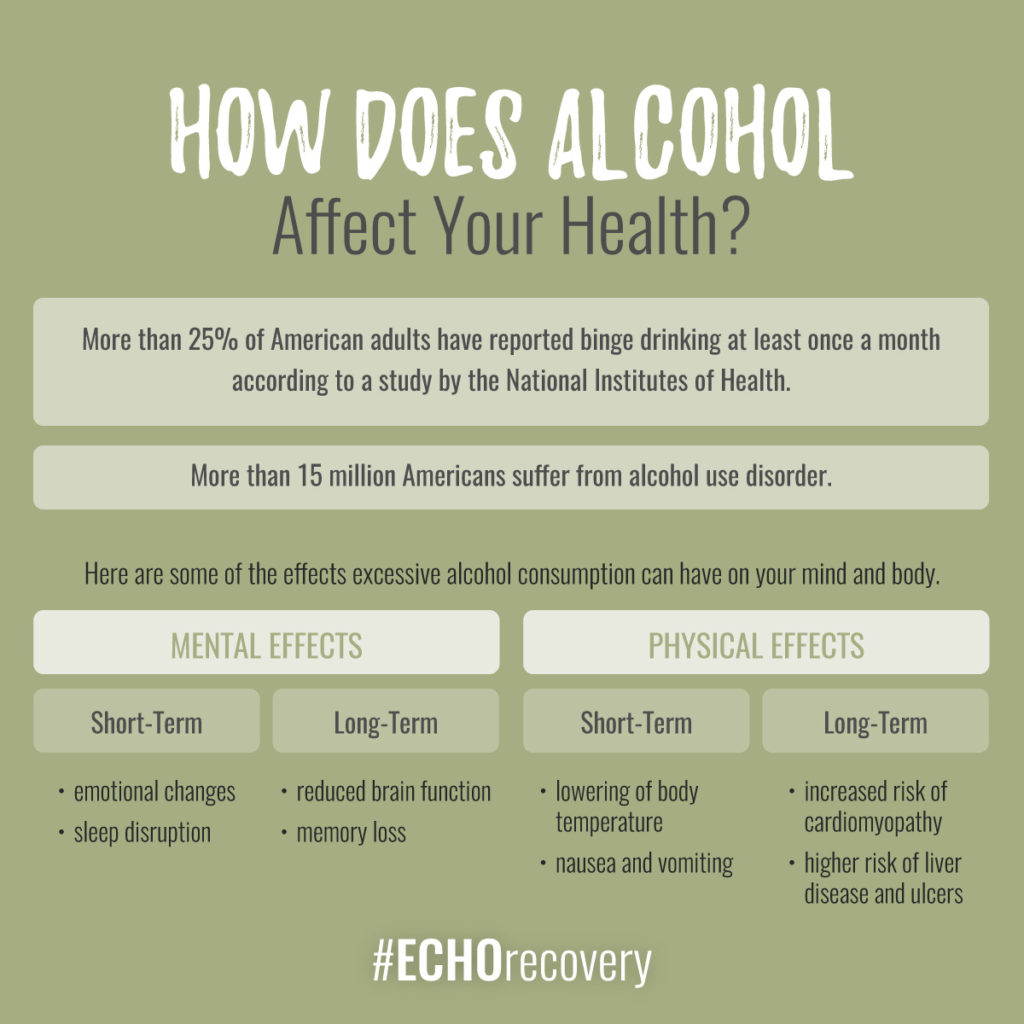 NIH stopped funding the study, formally known as The Moderate Alcohol and Cardiovascular Health Trial (aka MACH15), because the lead researcher and a few agency employees appeared to be “too cozy with the industry.” And by “industry,” we mean alcohol industry.
NIH stopped funding the study, formally known as The Moderate Alcohol and Cardiovascular Health Trial (aka MACH15), because the lead researcher and a few agency employees appeared to be “too cozy with the industry.” And by “industry,” we mean alcohol industry.