Thirteen years of war and the now ongoing Operation Freedom’s Sentinel and Operation Inherent Resolve in the Middle East have resulted in the highest number of veterans of foreign wars since the Vietnam era. These men and women who have made great sacrifices on behalf of our country come home and face a variety of problems, including:
- Lack of job opportunities
- Financial problems
- Homelessness
- Mental health disorders
Mental health issues – such as post-traumatic stress disorder (PTSD), anxiety disorders and other stress-related disorders, such as major depressive disorder (MDD) – are especially common due to traumatic wartime experiences. According to a 2015 VA report, around 24 percent of veterans returning from the Iraqi and Afghanistan wars suffer from PTSD. And about 30 percent of Vietnam War era veterans have had PTSD at some time in their lives.

PTSD Symptoms
The cause of PTSD is the body’s inability to come down from the flight or fight response and “gets stuck” or the person’s inability to move forward after going through a traumatic event. It can also manifest days, weeks or months down the road when something that reminds the veteran of the traumatic event triggers it.
Although diagnosis can only be done by a medical professional, here are some basic PTSD symptoms. These are not the only symptoms, there are others any of which could manifest or not, because not all PTSD sufferers are the same:
- Reliving the trauma, hallucinations or having intrusive thoughts about the traumatic event
- Hypervigilance, feeling unable to relax, always “keyed up” or on edge, irritability with no specific or rational cause, feelings of aggression, etc.
- Nightmares, sleep disturbances, insomnia, other sleep-related problems

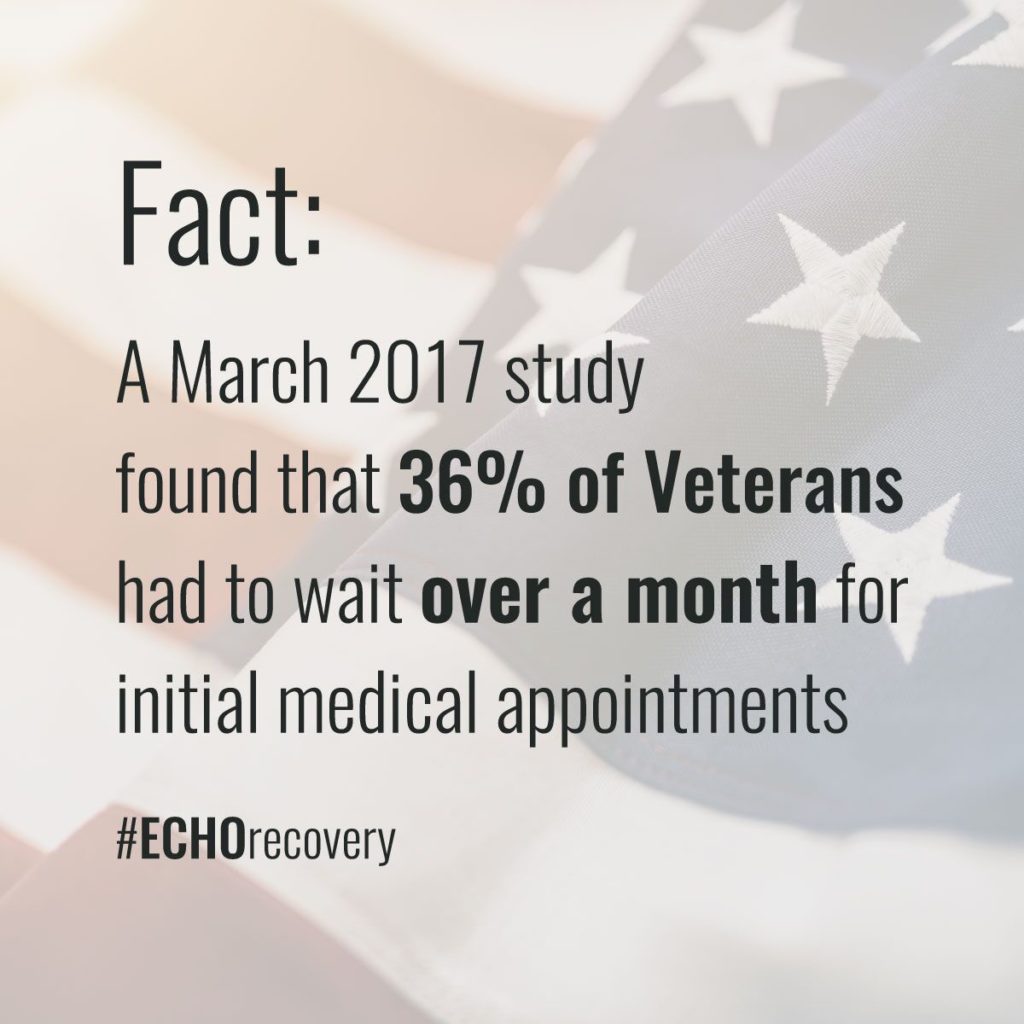
Because treatment of PTSD relies on a certain set of criteria to manifest and if not all those criteria are met, many a veteran is misdiagnosed and not given the proper treatment. In 2014, the VA system was woefully inadequate to properly serve the needs of our veterans. In 2017, after a $10 billion program was instituted to reduce wait times and get vets faster care, the wait times for first appointments and specialty care appointments has gotten better, however there is still a lot of room for improvement, especially in patient care.
Not only do vets still face fairly long wait times, but when they finally see a doctor they are often simply given prescription medications that have a host of potential side effects, including addiction.
Help for Vets with PTSD: Are We Too Reliant on Prescription Meds?
Trauma-related mental disorders are complicated to treat because each individual has different circumstances and varied responses to medication. Doctors need to be able to carefully diagnose the needs of each individual and try different treatment regimens to see what each patient responds best to, while minimizing harmful side effects. Many veterans also have co-occurring psychiatric issues, such as MDD, which occurs in about 50% of veterans diagnosed with PTSD.
But if it takes weeks and weeks for a vet to get one doctor’s appointment, and even then, getting the right diagnosis within a cattle-call system that still requires a lot of overhaul, then it’s very difficult for vets to get the individualized care they need. Simply giving them a prescription and then hoping for the best opens up vets to the very real risks of drug abuse and addiction, which only adds to the problems our vets face when they return home after serving our country.
The list of medications that can be used to treat mental illness in vets is extremely long (see below). What are the odds that the doctor is going to get it just right the first time when the patient is finally able to get an appointment?
Drugs that vets can be prescribed to treat PTSD-related symptoms fall into the following five categories.
Antidepressant Medications
These can be selective serotonin reuptake inhibitors (SSRIs) or selective norepinephrine reuptake inhibitors and are meant to balance the chemicals in your brain called neurotransmitters that affect mood and emotions. They should help improve mood, allow for better sleep and concentration.
- Amitriptyline (sold under brand names Elavil, Endep, Levate, others)
- Amoxapine (Asendis, Defanyl, Demolox, others)
- Bupropion or bupropion hydrochloride (Wellbutrin)
- Citalopram (Celexa, Cipramil)
- Clomipramine (Anafranil, Clofranil)
- Desvenlafaxine (Pristiq)
- Desipramine (Norpramin, Pertofrane)
- Doxepin (Deptran, Sinequan)
- Duloxetine (Cymbalta)
- Escitalopram (Lexapro, Cipralex)
- Fluoxetine (Prozac, Sarafem, others)
- Flurazepam (Dalmane, Dalmadorm)
- Fluvoxamine (Faverin, Fevarin, others)
- Imipramine (Tofranil)
- Maprotiline (Deprilept, Ludiomil, Psymion)
- Mirtazapine (Avanza, Mirtaz, Zispin, others)
- Nortriptyline (Sensoval, Aventyl, Norpress, others)
- Paroxetine (Paxil, Pexeva)
- Phenelzine (Nardil, Nardelzine)
- Protriptyline (Vivactil)
- Sertraline (Zoloft, Lustral)
- Trazodone (Oleptro, Trialodine)
- Trimipramine (Surmontil, Rhotrimine, Stangyl)
- Venlafaxine(Effexor)
- Vilazodone (Viibryd)
- Vortioxetine (Brintellix)
Anti-Anxiety Drugs
These work by increasing serotonin in the brain and decreasing dopamine levels,or by blocking the effects of norepinephrine, a stress hormone involved in the fight-or-flight response. thus relieving the symptoms of anxiety.
- Alprazolam(Xanax)
- Buspirone (Buspar)
- Chlordiazepoxide (Librium)
- Clonazepam (Klonopin)
- Diazepam (Valium)
- Estazolam (ProSom, Eurodin)
- Hydroxyzine (many names)
- Lorazepam (Ativan, Orfidal)
- Midazolam (Dormicum, Hypnovel, Versed)
- Oxazepam (Serax, many others)
- Temazepam (Restoril)
- Triazolam (Halcion, Trilam, others)
Antipsychotics
Usually used for bipolar disorder, these also work for anxiety, as they treat the hallucinations, aggression and flashbacks that may be a part of PTSD
- Aripiprazole(Abilify)
- Asenapine (Saphris)
- Fluphenazine (Prolixin, Modecate)
- Haloperidol (Haldol, others)
- Iloperidone (Fanapt)
- Loxapine (Loxapac, Loxitane)
- Lurasidone (Latuda)
- Olanzapine, sometimes in combination with fluoxetine (Zyprexa, Zypadhera or Symbyax)
- Perphenazine (Trilafon)
- Pimozide (Orap)
- Prochlorperazine (Compazine, Phenotil, others)
- Quetiapine (Seroquel)
- Risperidone (Risperdal)
- Thiothixene (Navane)
- Ziprasidone (Geodon, Zeldox, Zipwell)
Mood stabilizer
Also mostly used for bipolar disorder, these literally stabilize the mood swings caused by PTSD, by reducing overreaction to stressful situations.
- Carbamazepine(Tegretol, Carbatrol, others)
- Divalproex sodium(Depakote)
- Lamotrigine(Lamictal)
- Oxcarbazepine(Trileptal)
- Valproic acid(Depakene, Valproate)
Sleep Aids
These drugs help the brain reduce production of adrenalin and allow a person to go to sleep. Some of these are adrenergic blockers or beta blockers. These all also allow for a restful sleep.
- Butabarbital (Butisol)
- Eszopiclone (Lunesta)
- Prazosin hydrochloride (Minipress, Vasoflex, others)
- Ramelteon (Rozerem)
- Zaleplon (Sonata)
- Zolpidem (Ambien)
Bottom line: Simply medicating our vets, especially without giving them adequate follow-up care with their physicians, puts them at greater risk for problems stemming from prescription medication.
PTSD and Substance Abuse
Vets with PTSD are at greater risk for substance abuse in three ways:
- Some prescription drugs used to treat PTSD symptoms can be addictive.
- Vets who don’t get proper treatment for their symptoms may turn to alcohol and/or drugs to ease their symptoms on their own.
- Not enough or no psychotherapy or family support to help with PTSD symptoms.
While improper treatment can lead to addiction, many vets simply don’t get any care for their trauma-related illness, which can lead to:
- Withdrawal from or disinterest in previously enjoyed activities
- Job loss
- Financial difficulties
- Relationship problems
- Feelings of hopelessness, guilt or shame
- Homelessness
- Death

The suicide rate for veterans with PTSD is 50 percent higher than the national average. Overdoses are more likely to occur when substances are mixed (like prescription meds and alcohol), which is more likely to happen without proper doctor supervision.
Vets who have already developed a substance use disorder need treatment for both the addiction and their PTSD. This requires timely access to dual diagnosis professionals who can properly assess the individual’s needs and provide appropriate treatment.
Healthcare organizations that help vets with PTSD and addiction need to use a combination of therapy, medication and other proven treatment methods. The important thing is to ensure that each veteran gets the care he or she needs in a timely manner and with appropriate ongoing treatment.
How Can I Help Veterans with PTSD?
 Just as our servicemen and women have fought for freedom abroad, it is up to us to help fight for their well-being here at home. While there’s not a single solution to the problems that plague the VA medical system, our country can find solutions when concerned citizens take an interest.
Just as our servicemen and women have fought for freedom abroad, it is up to us to help fight for their well-being here at home. While there’s not a single solution to the problems that plague the VA medical system, our country can find solutions when concerned citizens take an interest.
The first step is engaging in open conversation about the issues and ways to solve them. We invite you to join the discussion online and share your thoughts on how we can better care for our soldiers when they return home.
Join The ECHO Recovery Movement By Donating Now
This was originally posted on May 15, 2018 and updated on August 8, 2019.

Experienced Chief Executive Addiction Recovery and Mental Health Professional
Business professional in the Addiction Recovery and Mental Health industry for the past 26 years. Caring, compassionate and strongly motivated to make a difference in the organizations I am affiliated with and welfare of the population we serve. Currently focused on advocating, educating and developing projects leveraging evidence based, real time technology to support individuals in recovery.




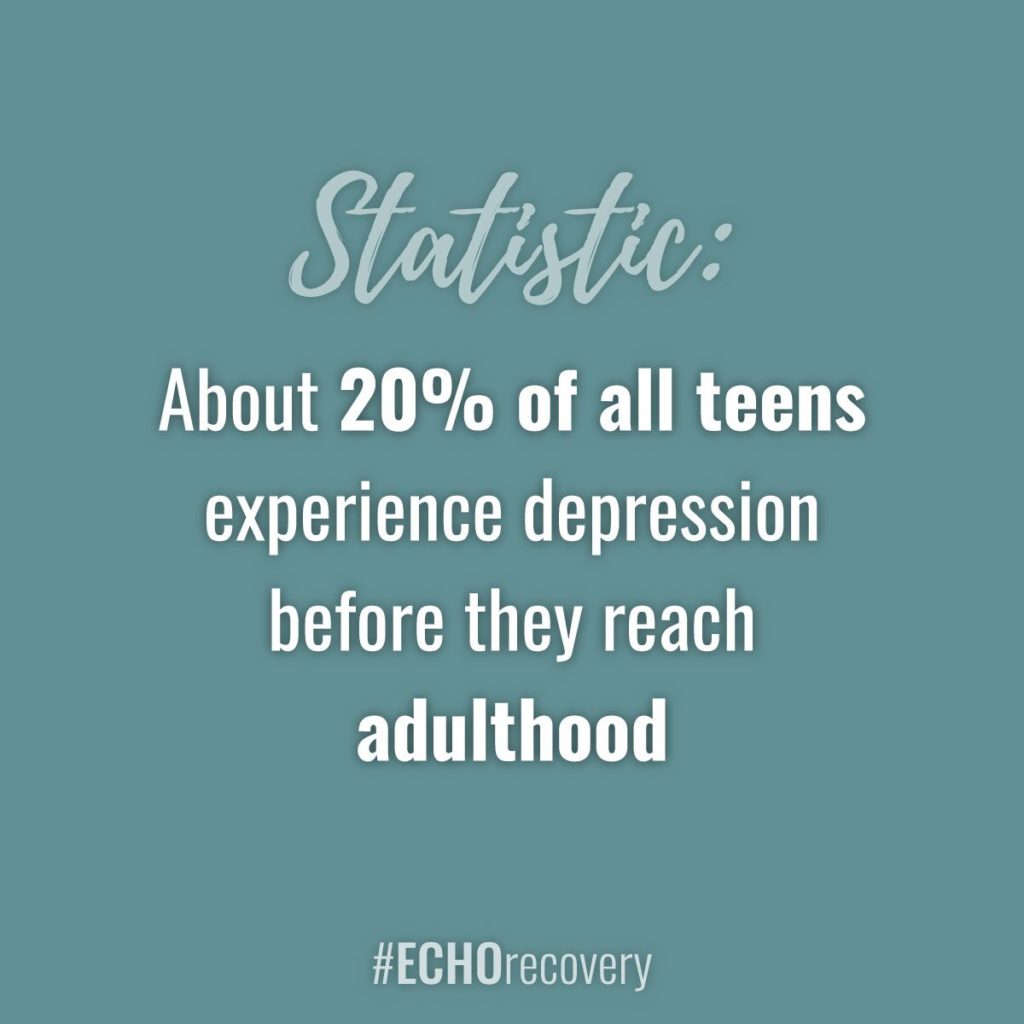 Because of the increased rates of depression and anxiety among today’s youth, our young people are more at risk of self-medicating and addiction than ever. More and more addiction treatment centers are offering programs focused on addressing anxiety in adolescents and young millennials to meet the needs of our current climate.
Because of the increased rates of depression and anxiety among today’s youth, our young people are more at risk of self-medicating and addiction than ever. More and more addiction treatment centers are offering programs focused on addressing anxiety in adolescents and young millennials to meet the needs of our current climate.