Recovering from an addiction is a complicated process that requires dedication and commitment for long-term, positive effects. It may be obvious that routines and lifestyles must be changed for your recovery to be successful. However, an area that you may not have considered changing is your social media use.
Unfortunately, there is a significant link between social media use and substance abuse addiction. Ironically, social media use is also linked to substance abuse recovery. It’s important to fully understand these links so you can start working on your recovery with fewer obstacles.
How Are Social Media and Addiction Linked?
The link between social media and addiction may not be obvious to you. Things like cute cat videos on social media do not have ties to substance abuse and addiction; however, there are still many connections between the two.
Glamorization and Normalization
Social media tends to glamorize drug and alcohol use. People can easily share photos and posts showing alcohol and drug use, making these activities appear fun, wild, and interesting. Though the average person’s post will not reach many people, celebrity posts create a lot of interaction and widespread viewing. Snoop Dog, Wiz, Khalifa, Drake, the Kardashians, Nina Dobrev, Cara Delevingne, and many other celebrities have photos of alcohol or drugs on their social media platforms that are followed by millions of people.
This effect can make people more likely to try commonly abused substances, which can then result in developing addictions. This glamorization is even more significant for teenagers, as roughly 81% of teens aged 12 to 17 use social media, much higher than the same figure for adults (67%). Their still-forming brains are more likely to be affected by what they see on social media, and they are more easily influenced into participating, either to impress peers or for attention.
Ease of Access
As mentioned, a vast portion of the world has access to social media. Therefore, social media makes a lot of things easily accessible to the public that are not normally so prevalent. Social media has been used to connect dealers with both current and potential customers. Substance dealers can use social media platforms to contact purchasers and reach a wider audience.
Location-based platforms like dating apps and Instagram make connecting dealers and those in their areas interested in buying the substances quite simple. Though the apps claim they attempt to prevent this use of their platforms, they are not effective at monitoring and shutting down violators.
 Mental Health Impacts
Mental Health Impacts
For some people, there is a link between social media and poor mental health. Most people only post positive aspects and filtered versions of their life, which can cause others to experience dissatisfaction with their own lives. This can spiral into sadness, depression, and isolation. These emotions may lead people to turn to substance abuse, which they’ve seen glamorized in other social media posts, to cope with their struggling mental health.
This is an important connection, as about half of individuals who develop substance abuse disorders will also have mental health disorders. This research also suggests that over 60% of adolescents in community-based substance use disorder treatment programs meet the criteria for mental illnesses.
Social Media as an Addiction
Finally, a major link between addiction and social media is the fact that it is possible to develop an addiction to social media itself. All addiction processes alter brain chemistry and damage reward pathways. A healthy reward pathway is activated when we experience something rewarding, winning a game, eating tasty food, or even having sex. At this point, dopamine is released, causing a positive emotional rush. This reward pathway intends to drive humans toward stimuli or behaviors that increase fitness and survival, while also driving them away from harmful stimuli that do the opposite.
Addiction damages this reward system and creates a dysfunctional reward pathway that is activated by addictive behavior. The reward system begins to function improperly, only becoming activated with the use of that substance or behavior. Further, less dopamine will be released with each experience, and the person will need to increase their exposure to get the same positive rush. This same type of damage occurs in any addiction process, whether the addiction is to drugs, gambling, sex, or even social media.
Can Social Media Worsen Addiction?
Not only can a person become addicted to social media, but social media use can also increase addictive behaviors and make an active addiction worse. A person that overuses social media is also more likely to have brain impairments like those seen with a clinical addiction. Decision-making skills are decreased, and heavy social media users are more prone to poor choices.
Since social media addiction affects the brain’s reward system, a person may search for new ways to achieve a dopamine rush. Since their decision-making skills are impaired, some may turn to drugs to experience the dopamine rush they are no longer experiencing with social media alone.
Social Media and Addiction Recovery
Recovering from an addiction is a massive undertaking that requires making deliberate choices and utilizing any resources. With that in mind, social media can be both a hindrance and a support to recovery, depending on how it is used. You must be able to remain vigilant about your social media use and how it is affecting you during that specific time in your recovery process.
Identifying how social media influenced you during active addiction can help you positively alter your habits. Using social media while in recovery for addiction is a delicate process and may be aided with the help of a professional. Let’s take a look at how social media can help and hurt your recovery.
Hindrances to Recovery

Negative Self Image
As mentioned before, social media is full of people posting about the positives in their lives, like job promotions, relationships, and fun vacations. However, these posts often leave out all the less than glamorous parts behind the positives. A job promotion may have followed many long days at their job, a good relationship may have been found after a string of bad dates, and the vacation may have been the first one they’ve taken in many years.
Unfortunately, it is difficult to remember these negatives when confronted with post after post of other people’s lives working out well, and this can result in feelings of inadequacy, envy, and the fear of missing out (FOMO). One may choose the comfort and familiarity of their addiction instead of these negative emotions, making recovery more difficult.
Sleep Deprivation
Those that struggle with addiction are far more likely to have a sleep disorder than the general population. Disturbances in sleep patterns and cycles can increase the likelihood of relapse, as your brain and body lose out on the healing that occurs during sleep. Overusing social media can decrease the time you have available for sleep and make recovery a steeper hill to climb.
Depressing/Harmful Content
We know depression can be a significant contributor to addiction. Unfortunately, being bombarded with information that hurts your mental health while scrolling social media can further hinder recovery. In addition, social media exposes you to many more people and situations than you would experience in person. Some of these people will have bad intentions and can spread their own negative emotions to you via online interactions like cyberbullying (abusive messages, images, or posts directed at an individual). Maintaining a positive headspace will be next to impossible if you’re bombarded with negative content on your social media.
Advantages to Recovery
Family and Friends
Social media can be used to maintain contact with family and friends. Having a strong support system made up of the people that care for you is important for recovery and preventing relapse. These people can quickly provide support by liking and commenting on your content. Preventing feelings of isolation will help with the confidence it will take to follow through with recovery.
Online Recovery Forums/Groups
Social media provides access to millions of people that you will never see in person. Some of those people will have had similar experiences to yours and they may openly post about their struggles and what helped them recover. Seeing their success stories may be bolstering enough for you to aid your recovery. There are also many online groups created to offer support for those undertaking their recovery process.
These online groups offer some anonymity that may help you feel more comfortable with sharing and confiding your story in the support group. Finding support in a community is vital to lowering the chance of relapse and creating habits that will result in lifelong sobriety.
Apps Created for Recovery
Support programs have taken advantage of social media and created apps to aid with your recovery. There is an FDA-approved app for substance abuse treatment, Pear reSET-O, that offers a 90-day behavioral program for adults, available with a prescription from your doctor. There are also many different apps available without a prescription that can help track your sobriety, manage cravings, find treatment providers in your area, create an online community specifically for those going through recovery, and offer inspirational content about addiction and recovery.
Seek Addiction Treatment and Recovery

Ultimately, treatment and recovery for addiction is a massive undertaking that frequently requires that you seek help from outside sources. A lack of support likely had a hand in the addiction, so leaning on a support system—no matter the source—may be a valuable tool to help pull you out. I believe social media can help, but it must be used correctly, in conjunction with other resources. As you can see, our addiction recovery community uses a few social media platforms, and they can be an excellent resource when used correctly.

Experienced Chief Executive Addiction Recovery and Mental Health Professional
Business professional in the Addiction Recovery and Mental Health industry for the past 26 years. Caring, compassionate and strongly motivated to make a difference in the organizations I am affiliated with and welfare of the population we serve. Currently focused on advocating, educating and developing projects leveraging evidence based, real time technology to support individuals in recovery.

 Mental Health Impacts
Mental Health Impacts













 According to fMRI scans run by Hal Hershfield of the
According to fMRI scans run by Hal Hershfield of the  At ECHO Recovery, we are committed to educating the public about recovery and all the latest science behind it, including future-self visualization as a method of motivating a person to seek help with substance use disorder. We are also passionately fighting the stigma of substance use disorder and its negative effect on those in recovery.
At ECHO Recovery, we are committed to educating the public about recovery and all the latest science behind it, including future-self visualization as a method of motivating a person to seek help with substance use disorder. We are also passionately fighting the stigma of substance use disorder and its negative effect on those in recovery.
 Recovering addicts experience acute withdrawal syndrome as their bodies try to adapt to the sudden absence of drugs. Withdrawal symptoms are caused by changes happening in your body as it tries to adjust. The symptoms caused by these physical changes are physical ones, often causing intense bodily discomfort, pain, and complications.
Recovering addicts experience acute withdrawal syndrome as their bodies try to adapt to the sudden absence of drugs. Withdrawal symptoms are caused by changes happening in your body as it tries to adjust. The symptoms caused by these physical changes are physical ones, often causing intense bodily discomfort, pain, and complications.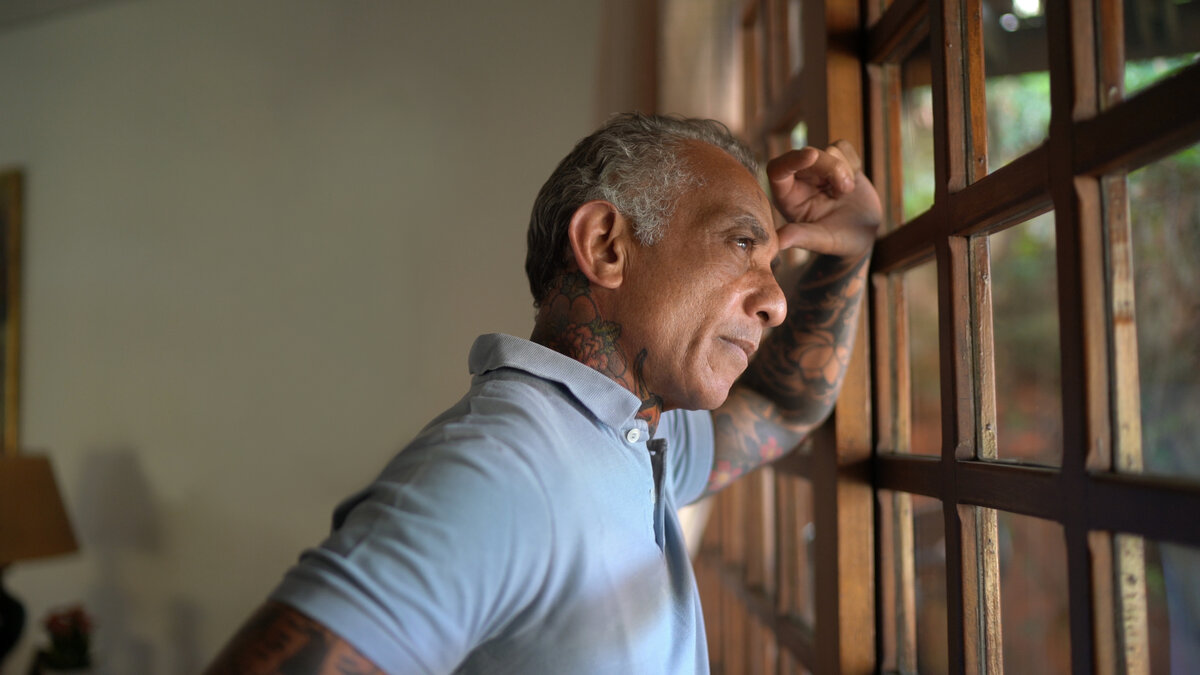 Unfortunately, there is no specific PAWS timeline. Just as there are many factors involved in determining who experiences PAWS, what symptoms they have, and how extreme the symptoms are, these same variables also affect how long PAWS will persist. When PAWS first sets in, it often feels like a roller coaster, with moods and feelings changing from minute to minute. Gradually, the time between changes gets longer. Later in the process, there may be weeks between symptoms. However, it’s important to be aware that even as the time between symptoms grows longer, bad episodes may still last for several days at a time.
Unfortunately, there is no specific PAWS timeline. Just as there are many factors involved in determining who experiences PAWS, what symptoms they have, and how extreme the symptoms are, these same variables also affect how long PAWS will persist. When PAWS first sets in, it often feels like a roller coaster, with moods and feelings changing from minute to minute. Gradually, the time between changes gets longer. Later in the process, there may be weeks between symptoms. However, it’s important to be aware that even as the time between symptoms grows longer, bad episodes may still last for several days at a time.
 It can be difficult to navigate PAWS, especially because it is impossible to predict exactly what symptoms will occur. Having strong family support can make the process more bearable, while seeking the help of counselors and therapists can help mitigate the symptoms and help reduce the chances of relapse.
It can be difficult to navigate PAWS, especially because it is impossible to predict exactly what symptoms will occur. Having strong family support can make the process more bearable, while seeking the help of counselors and therapists can help mitigate the symptoms and help reduce the chances of relapse.
 When we are disconnected from our future selves, we are less likely to consider the impact that today’s actions have on our future. Our biases towards thinking in terms of the present make immediate gratification a more tempting option. We can see, feel, and taste the impact of our decisions in the present, but their effects on our future selves are a lot less tangible. For many of us who have struggled with addiction and substance abuse disorders, this is an all too familiar mindset.
When we are disconnected from our future selves, we are less likely to consider the impact that today’s actions have on our future. Our biases towards thinking in terms of the present make immediate gratification a more tempting option. We can see, feel, and taste the impact of our decisions in the present, but their effects on our future selves are a lot less tangible. For many of us who have struggled with addiction and substance abuse disorders, this is an all too familiar mindset. It isn’t that difficult to see how a disconnection to the future version of ourselves contributes to the choices that many of us made that lead us down the path of substance abuse. The immediate gratification of getting high or having that drink was much more tangible than the idea that our future self might end up in a rehab facility, especially when our mind thinks of our future self in the same way it views a stranger. Why would we prioritize the health and happiness of someone we aren’t connected to above the happiness and immediate gratification of this real-time version of ourselves?
It isn’t that difficult to see how a disconnection to the future version of ourselves contributes to the choices that many of us made that lead us down the path of substance abuse. The immediate gratification of getting high or having that drink was much more tangible than the idea that our future self might end up in a rehab facility, especially when our mind thinks of our future self in the same way it views a stranger. Why would we prioritize the health and happiness of someone we aren’t connected to above the happiness and immediate gratification of this real-time version of ourselves? The path of recovery requires that we not only take each 24-hour day, minute by minute but also that we envision a future for ourselves that is full of the things that we define as success and the love and joy of our friends and family. Our journey is a
The path of recovery requires that we not only take each 24-hour day, minute by minute but also that we envision a future for ourselves that is full of the things that we define as success and the love and joy of our friends and family. Our journey is a 





